Abstract
Background. Haploidentical related donors (HIDs) are attractive donors for patients with severe aplastic anemia (SAA) because they are readily available for nearly all the patients. Bone marrow transplant (BMT) using post-transplant cyclophosphamide (PTCy) has been shown effective to cross the immune barriers between the recipients and their HIDs. Short-term low dose of methotrexate (ST-MTX) has long been adopted either alone or combined with calcineurin inhibitors to get across the immune barrier in hematopoietic stem cell transplant (HSCT).
Aim of the study. We presented the outcome of 15 patients with SAA who underwent haploidentical transplant (HIT) using T-cell-replete peripheral graft and combination of PTCy with ST-MTX.
Patients and grafts. We analyzed the medical records of 15 patients with SAA between Jan 2015 and July 2017. The transplants were either upfront (8/15) or rescue treatment (7/15). The median age of the patients was 16 (range 5-39) years and 66.7% (10/15) were male. All the patients received granulocyte colony-stimulating factor (G-CSF) mobilized peripheral graft from haploidentical related donors. The median mononuclear cells (MNCs) was 12.4 × 108 cells/kg recipient ideal body weight (IBW) with the range of (7.0-22.0) × 108 cells/kg, the CD34+ cell was 7.5 × 106 cells/kg with the range of (5-23) × 106 cells/kg and the CD3+ cells was 2.7 × 108 cells/kg with the range of (1.8-5.0) × 108 cells/kg.
Conditioning regimen and GvHD prophylaxis. We used a TBI-free transplantation platform named FBC+PTCy/ST-MTX. Fludarabine was administered at 40 mg/m2 IV daily for 5 days. Busulfan was delivered in a total dose of 6.4mg/kg. Cyclophosphamide was given 14.5 mg/kg daily for 2 days. PTCy was administered at 60mg/kg/day IV on days +3 and +4 post-transplant. Low doses of MTX were delivered on days +1, +2 and +5 post-transplant at 15mg/m2, 10mg/m2 and 10mg/m2. Cyclosporine was given from day +6 through day +180 with the target through level 150~180ng/ml and then was tapered until 12 months post transplant. Mycophenolate mofetil (MMF) was given from day +6 to +35 days for the first 3 patients and then was eliminated for the following patients.
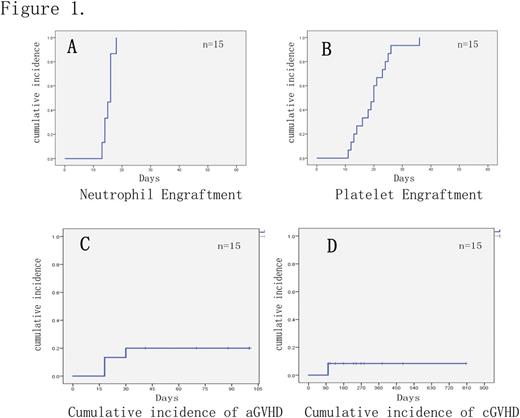
Results.Neither primary nor secondary graft failure (GF) was seen in this study. Neutrophil engrafted at 15 days (range, 13-18 days). Platelets engrafted at 19 days (range, 14-36 days) and recovered over 100 × 109/L at 38 days (range, 14-77 days). The time to total lymphocytes recovery over 0.5 × 109/L for 3 consecutive days was 34 days (range, 25-72 days). The accumulated engraftment of neutrophil and platelets were both 100% at +40 days. (Figure 1-A, B.)
The cumulative incidence of aGvHD at 100 days was 20.0%(3/15). Two patients had grade I skin aGvHD and the other one had grade II skin aGvHD. No grade III-IV aGvHD was seen. 12 patients were evaluable for the incidence of cGvHD and none of them developed moderate or sever cGvHD with a median of 150 (102-806) days post transplant. (Figure 1-C, D.) During the follow-up, one patients had skin cGvHD and received systemic therapy with corticoid. The treatment was discontinued after 8 months post transplant. All 3 patients, who survived beyond 12 months post transplant at the end of our follow-up, were off immunosuppress.
With a median follow-up of 230 days (range 41-806 days), all the patients are alive. They are transfusion independent with karnofsky performance status scale (KPS) scores 100.
Conclusion.This study shows that haploidentical related transplant can be successfully applied using T-cell-repleted peripheral grafts. ST-MTX may facilitate PTCy to achieve a stable engraftment with a minimal risk of GvHD in HIT for patients with SAA. Our approach should expand the donor pool for patients with SAA.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal